Pain caused by arthritis can be distressing, unpleasant and sometimes debilitating. It affects millions each year and prevents them from living life to its fullest. Here you will find information to help you better manage arthritis pain symptoms and improve your quality of life.
Learn more about arthritis pain and how to manage it to live well with the condition.
What is pain?
Pain is something you feel physically and emotionally – it is not pleasant and is due to a perception of real or potential damage to your body.
The amount of pain a person experiences is not always equal to the amount of damage or harm to their body. Someone can experience pain without tissue damage or can have tissue damage without pain.

How does your body process pain?
While pain may start at different places in your body, all pain is perceived and processed by your brain. Pain is your body’s warning system alerting you to harm.
A pain signal travels through your nerves (usually – but not always – starting from those nerves closest to the source of harm), up your spinal cord to your brain. Your brain then interprets the pain signal based on its intensity and location, as well as a variety of other information such as your surroundings, previous injury experience, your beliefs, your emotional state, and many other factors. You feel the pain after your brain has processed all of this information.
Pain is personal
When your brain processes a pain signal, it considers many factors that are personal to you. As a result, you feel pain differently from everyone else – even from people who may have the same disease or injury as you. Just like your experience with arthritis can be very different from someone else’s, the same goes for the pain you experience. This also means that pain treatments (including medications and other interventions) that work for one person may not work for another or may work differently.
There is a strong mind-body connection in pain. Your emotions and thoughts play a large role in how you experience pain, and pain can affect all aspects of your life.
Types of pain
Acute pain is short-term pain that serves to protect you and prevent more damage by causing you to change your behaviour. Some examples are pain caused by an injury, surgery, or a toothache.
When our body is injured or damaged, our nerves communicate this message to our brain. The brain then responds by sending a message to our body to react. Acute pain helps us protect the injury to our bodies and prevent further damage. Usually, this pain goes away when the damaged part of your body heals or no longer needs protection, or the unpleasant stimulus has been removed.
 Chronic pain (also called persistent pain or long-term pain) lasts longer than acute pain, typically for more than three months. People who live with chronic diseases often live with chronic pain. This type of pain does not necessarily mean that damage is occurring – even though it might feel that way. While chronic pain is not fully understood, we know that it is sometimes caused by a problem with one or more nerves and the way they send pain messages to the brain.
Chronic pain (also called persistent pain or long-term pain) lasts longer than acute pain, typically for more than three months. People who live with chronic diseases often live with chronic pain. This type of pain does not necessarily mean that damage is occurring – even though it might feel that way. While chronic pain is not fully understood, we know that it is sometimes caused by a problem with one or more nerves and the way they send pain messages to the brain.
Some people with chronic pain also experience ‘pain sensitization,’ which is basically your body turning up the volume on your pain. This often leads to a heightened sensitivity to pain and touch. In chronic conditions such as arthritis, areas of the brain that send and receive danger signals become more sensitive over time. The more the brain processes pain, the more perceptive it becomes until it remains in a state of heightened alert and response, which can distort the experience of pain.
Our thoughts, emotions, and activity levels can increase the sensitivity of the nervous system, leading to pain being felt more often and more intensely. Although there is currently no cure for chronic pain, we can treat chronic pain by learning how to manage it.
Both acute and chronic pain are influenced by biological, psychological, social and environmental factors. Understanding the differences between acute and chronic pain, as well as the transition from acute to chronic pain is the first step in addressing ongoing pain.
When you live with chronic pain, you are rarely entirely without pain, but you will have good days when you feel less pain and bad days when you feel more. Pacing yourself and your activities and tracking how you feel from day to day will help you learn to understand your pain. These approaches will also help you maintain a schedule so you can better predict what your days with pain will be like.
Where does arthritis pain come from?
While we continue to study the mechanisms of pain in the body, we know that most arthritis pain typically arises from one or more of these sources:
 Inflammation – pressure on nerves in and around joints due to swelling
Inflammation – pressure on nerves in and around joints due to swelling- Joint damage – damage to tissues in and around joints, nerves and/or surrounding tissues due to injury or prolonged inflammation
- Pain sensitization – prolonged pain can lead the body to send pain signals to the brain, even in the absence of a specific ongoing pain source
Some of the factors that can contribute to your experience of arthritis pain – how it feels to you – include:
- Physical activity – joint strain from either excessive or insufficient physical activity
- Muscle tension – muscles may be tense because of stress, insufficient physical activity or poor posture
- Fatigue – exhaustion from managing chronic pain, lack of mobility or poor sleep due to pain can impact coping skills
- Anxiety and/or depression – stress and low mood can increase the perception of pain and decrease your capacity to cope
- Too much focus on pain – strong body-mind connection means that focusing on your pain can increase pain sensitivity and reduce coping skills
- Attitude and belief system – your outlook on life can directly impact the level of pain you experience, and your ability to cope with it
- Social environment and support – people who feel the support and understanding of strong social networks feel less overwhelmed and better able to cope with their pain than people without that support
The best pain management results often involve a combination of ongoing self-management and medical treatment. This multi-modal approach to treatment includes physical, psychological, pharmacological (medication-based) and preventative strategies.
The arthritis pain cycle
Chronic pain may be affected by the following:
- Physical problems caused by injury, disease or surgery
- Tense muscles (which may actually be your body’s reaction to protect injured joints)
- Psychological stress
- Depression or other negative emotions and feelings
- Fatigue
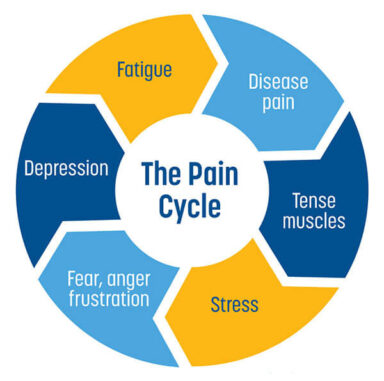
Your experience of pain is influenced by the factors above – as they feed into one another, they can prolong and amplify your pain. If you are able to break the cycle by addressing even one or two of the factors, it is possible to achieve some significant relief from your pain.
Additional contributing factors
 While chronic pain can increase stress levels that play a role in the pain cycle, stressful experiences such as trauma or discrimination can also impact the intensity, severity and duration of pain. Research has shown that chronic stress resulting from a history of trauma or ongoing experiences of discrimination such as racism can have a negative impact on our bodies and can contribute to pain and inflammation.
While chronic pain can increase stress levels that play a role in the pain cycle, stressful experiences such as trauma or discrimination can also impact the intensity, severity and duration of pain. Research has shown that chronic stress resulting from a history of trauma or ongoing experiences of discrimination such as racism can have a negative impact on our bodies and can contribute to pain and inflammation.
When our body is in continual fight-or-flight mode, it triggers our nervous system to be on the lookout for danger, which can lead to an increased sensitivity to pain. The chronic stress caused by experiences of trauma or discrimination can impact the neuroendocrine system and lead to dysregulation of the stress hormone cortisol.
Stress hormones can have helpful short-term effects by keeping us alert in dangerous situations, such as increasing our heart rate so blood and oxygen will move quickly throughout the body. Additionally, stress hormones can inhibit inflammation and slow down digestion so that energy is reserved for our important heart and brain functions.
In the long-term, however, high levels of stress hormones can impact pain experiences by negatively feeding into the pain cycle. Elevated levels of cortisol in the circulatory system for longer periods of time can lead the body to become cortisol resistant and send our immune systems into overdrive, leading it to attack cells and tissues that aren’t a threat.
Trauma-informed and anti-discriminatory healthcare can play a role in helping to address these issues, but just being aware of how chronic stress can contribute to your experience of pain can help you take control of your symptoms. A multi-level approach to pain management that addresses physical, psychological, and social factors is important.
An important part of arthritis pain control is self-management. This refers to activities and supports that you can use on your own to reduce joint pain. The following provides information, tools and strategies to help you take an active role in arthritis pain relief.
Physical Activity & Exercise
 Arthritis may cause you to avoid physical activity for a number of reasons, including fear of making your arthritis worse, because movement is painful, or because you are tired. Although it may be difficult to stay active when living with joint pain, maintaining regular physical activity can be an important part of pain control and retraining the brain to experience pain less intensely.
Arthritis may cause you to avoid physical activity for a number of reasons, including fear of making your arthritis worse, because movement is painful, or because you are tired. Although it may be difficult to stay active when living with joint pain, maintaining regular physical activity can be an important part of pain control and retraining the brain to experience pain less intensely.
Physical activity can release endorphin hormones, which reduce stress and pain. Exercise can also stimulate the release of hormones that increase feelings of happiness and wellbeing (such as serotonin and dopamine). Physical activity overall helps improve strength, range of motion, sleep, and energy, which can have a positive impact on our experience of pain.
When we avoid doing activities that we believe will result in pain, we can reinforce the brain’s perception that these activities are associated with danger and pain. However, consistent participation in safe physical activity can help retrain the brain. When taking part in physical activity, make sure to pace yourself by balancing periods of activity with periods of rest. Instead of going for very long, high-endurance walks or hikes, consider going for shorter and more frequent walks throughout the day.
There are many benefits to physical activity and exercise if you are living with arthritis. A regular routine can increase your strength, your energy and your flexibility. Research shows that physical activity helps people manage their joint pain and can also relieve stiffness, improve energy, and make your everyday activities easier to do. It can also help with weight management, which may play a role in reducing pain for some people.
Getting started
There are a few basic principles that will help you get started:
- Consult with your health care team about physical activity and exercise that will work for you given your personal situation. A physiotherapist can help develop a therapeutic exercise program unique to your needs.
- Start slowly and pace yourself
- Find activities you enjoy since you are more likely to stick with these in the long term
- Exercise with a friend
- Remember to warm up before exercise and cool down afterwards
Setting achievable goals related to physical activity will help you gain some control over your pain. Below is a list of resources to help you get moving.
Exercise videos
*Please consult with your healthcare provider before starting any new exercise
Exercises for the whole body
Follow along with these exercise videos that will help you build overall strength and flexibility.
Exercises for specific joints
These videos will teach you exercises to help relieve symptoms of arthritis in particular areas of the body.
- Exercises for Osteoarthritis of the Hips and Knees
- Exercises for Osteoarthritis of the Shoulders
- Arthritis Advice: Hand Exercises
Guidance on physical activity and exercise – videos
Learn how to become more active and practice exercise safely with these helpful videos.
- Arthritis Advice: Walking
- Arthritis on the Move: Nordic Walking
- Arthritis Talks webinar: Managing Arthritis with Physical Activity and Assistive Devices
Guidance on physical activity and exercise – written resources
These written resources will help you learn more about safe physical activities for arthritis and how to protect your joints
- Articles on Physical Activity and Exercise
- External Resource: Canadian 24-Hour Movement Guidelines
- Information about GLA:D Canada: www.gladcanada.ca *Please note that some programs may have a cost
 Eating Well
Eating Well
While unfortunately there is no miracle diet for arthritis, food can play a significant role in arthritis pain control. What we eat can impact inflammation as well as our energy levels, mood, and weight, which are all factors in how we experience arthritis pain. For people living with gout, diet is particularly important when it comes to managing symptoms.
Additionally, research has shown that for people living with knee OA and carrying excess weight, a reduction in weight by 10% or more can have a significant impact on joint pain, mobility and function. A diet rich in vegetables, fruits, whole grains, lean proteins and healthy fats can help reduce inflammation and manage weight. Keep in mind portion sizes by using the balanced plate approach: make 1/2 your meal vegetables or fruit, 1/4 whole grains, and 1/4 protein foods, choosing plant proteins more often.
Visit the resources below to learn more about how food can help you take control of your arthritis symptoms.
Learning the basics of nutrition for arthritis
Recipes and meal planning
- Recipes for Healthy Eating
- Taming Arthritis: A Guide to Anti-Inflammatory Eating (article)
- Healthy Eating and Nutrition for Arthritis (PDF)
- The truth about nightshades and arthritis (article)
Heat/Cold Therapy
Heat and cold therapies can be helpful for short-term pain relief. Cold therapy can be used to reduce pain, inflammation and swelling if your joints are hot and swollen. Heat therapy is helpful for relaxing muscles and improving circulation. Be sure to protect yourself by placing a cloth or towel between the heat/cold treatment and your skin.
 Mindfulness Meditation and other Mind-Body Approaches
Mindfulness Meditation and other Mind-Body Approaches
Our brain is a powerful tool we can use to help control our experience of pain. Of course, pain isn’t “just in our heads,” but science has shown that techniques such as mindfulness meditation, cognitive behavioural therapy, distraction, and visualization may help reduce the intensity of the pain we experience.
Below are some resources on mind-body approaches you can try.
- Mindfulness meditation
Mindfulness meditation is a practice that research has shown may have potential benefit for long-term pain management. While it can’t take away pain, it can help us reframe our response to pain so that we experience it less intensely. Mindfulness exercises help individuals focus their mind and body in the moment. Instead of paying attention to unpleasant thoughts about pain, individuals can focus on their breathing, body sensations and relaxing their body. Mindfulness helps us think about pain with less fear and more acceptance, allowing us to live a good, healthy lifestyle, despite having pain. - Progressive muscle relaxation
Progressive muscle relaxation involves working systematically through the different muscle groups in your body and tensing them as you breath in, then relaxing them as you breath out. This practice invites you to pay attention to how your muscles feel once tension is released and they are relaxed.Progressive muscle relaxation can help with pain relief because we often unconsciously tense our muscles around a sore area, which can make the pain worse. Learning to notice the different feelings of tension and relaxation in our muscles can help us recognize when we are unconsciously tensing up and what we can do to relax our muscles.Anxiety Canada has an excellent resource on progressive muscle relaxation, which includes a guided recording that you can follow: How to Do Progressive Muscle Relaxation. - Visualization
Visualization or guided imagery is a short-term pain management strategy that uses the power of the mind to imagine specific positive scenarios that may help calm down the mind and relax the body. Visualization is about redirecting your attention to a positive memory or sensation, which may trigger the release of endorphins – your body’s natural pain relievers.Examples include remembering all the details about a favorite picture (where it was taken, what happened, etc.) or imagining yourself picking your favourite fruit, carefully choosing it, examining its texture, how it smells, cutting it up, eating and tasting it. The Hospital for Sick Children (Sick Kids) and Cassie + Friends partnered to create an excellent series of audio meditations that include visualization exercises. While some are more directed towards youth, most of the videos are appropriate for all ages: Audio Meditations. - Distraction
Like visualization, distraction shifts your attention from pain to another topic, taking advantage of the fact that your mind has trouble focusing on more than one thing at a time. This is a short-term pain management strategy. The goal is to occupy your brain with a detailed task.Some examples of distraction might include counting in multiples of an odd number, remembering all the words of a song, reciting the alphabet backwards, etc. Remember not to ignore your pain completely since it also protects you from harm. Emerging research has shown that virtual reality may be an effective tool in distraction from pain. To learn more, visit our article on Virtual Reality and Pain. Also, the Hospital for Sick Children (Sick Kids) and Cassie + Friends partnered to create an excellent series of audio meditations that include distraction exercises. While some are more directed towards youth, most of the videos are appropriate for all ages: Audio Meditations.
Additional Resources:

Assistive Devices and Joint Protection
Taking action to protect your joints and minimize joint strain can help reduce arthritis pain and make daily tasks easier. Assistive devices can include practical tools and gadgets, mobility aids, medical equipment or assistive technologies that help you perform activities of daily living more easily, such as cooking, walking, or getting dressed. There are also physical joint protection techniques you can use to avoid putting weight on your joints in awkward positions and to reduce strain.
Visit the resources below to learn more about what you can do to help relieve joint pain.
Written resources
Videos
- Life Hack Videos: Tips and tricks for doing daily tasks with greater ease and less pain, including dressing, cooking with pots, grasping and turning, washing and bathing, and more.
- Arthritis Talks Webinar: Managing Arthritis with Physical Activity and Assistive Devices
In the Workplace
- Workplace Accommodations for People with Arthritis
- Joint Matters at Work Podcast: Lifting, Driving, Work Stations
Pain Management Programs and Clinics
There are a number of different pain management programs across Canada, including self-directed programs as well as programs offered through medical services that require a referral from your doctor. Some services are available online or over the telephone and others are in-person. In this section, you will find information about multi-week pain management programs, health coaching programs where available, and other regional pain resources. Select your region to learn more about programs and supports offered in your community. If there are any programs or resources you feel are missing, please let us know at [email protected].
Access from Anywhere: Pain Trainer Program: a self-guided interactive, online program for pain management developed in collaboration between Northwestern University, Duke University, and the University of Melbourne (free program that requires registration)
Province-wide
- Arthritis Rehabilitation and Education Program: offers free physiotherapy, occupational therapy, and social work services to people living with arthritis, as well as group education workshops
- Online Self-Management Program: includes one-to-one health coaching, online group-based workshops, and a six-week online program on Progress Over Pain
Regional
Erie St. Clair
- Chronic Pain Workshop Series: Available in English and French. Call toll free 1-855-259-3605.
- Health Centres and Programs for Indigenous Peoples
South West
- Living a Healthy Life with Chronic Pain (South West Region): A free 6-week chronic pain self-management program
- Health Centres and Programs for Indigenous Peoples
Waterloo Wellington
- Active Living with Chronic Pain Toolkit: self-directed learning with phone support
- Taking Charge of Chronic Pain: free 6-week workshop series
- Health Centres and Programs for Indigenous Peoples
Hamilton Niagara Haldimand Brant
- TakeControlTakeCharge: offers a six-week Chronic Pain Self-Management Workshop
- Health Centres and Programs for Indigenous Peoples
Central West
- Living a Healthy Life with Chronic Pain: free 6-week chronic pain self-management program
- Health Centres and Programs for Indigenous Peoples
Mississauga Halton
- Living a Healthy Life with Chronic Pain: free 6-week chronic pain self-management program
- Health Centres and Programs for Indigenous Peoples
Toronto Central
- Chronic Pain Self-Management Program: free 6-week program
- Peer Health Coaching: free support by telephone
- Health Centres and Programs for Indigenous Peoples
Central
- Living a Healthy Life with Chronic Pain: free 6-week chronic pain self-management program
- Health Centres and Programs for Indigenous Peoples
Central East
- Living a Healthy Life with Chronic Pain: free 6-week chronic pain self-management program
- Health Centres and Programs for Indigenous Peoples
South East
- Living Well with Chronic Pain: free 6-week chronic pain self-management program|
- Health Centres and Programs for Indigenous Peoples
Champlain
- Living a Healthy Life with Chronic Pain: free 6-week chronic pain self-management program
- Health Coaching: free support by telephone
- Health Centres and Programs for Indigenous Peoples
North Simcoe Muskoka
- Living a Healthy Life with Chronic Pain: free 6-week chronic pain self-management program
- Health Services for Indigenous Peoples
North East
- Living a Healthy Life with Chronic Pain: free 6-week pain self-management program
- Health Centres and Programs for Indigenous Peoples
North West
Province-wide
- Association québécoise de la douleur chronique
- My Pain Management
- First Nations of Quebec and Labrador Health and Social Services Commission: Health and Wellness Services – information about programs and services for First Nations communities in Quebec
Regional
Programs offered by regional CIUSSS and CISSS require a referral from your doctor:
- Montreal: Programme Douleur Chronique
- Centre intégré universitaire de santé et de services sociaux de la Mauricie-et-du-Centre-du-Québec: Clinique de gestion de la douleur
- Centre intégré de santé et de services sociaux de Chaudière-Appalaches : Gestion de la douleur
- Centre intégré de santé et de services sociaux du Bas-Saint-Laurent : Douleurs chroniques
- Centre intégré universitaire de santé et de services sociaux du Saguenay—Lac-Saint-Jean : Douleur chronique
- Centre intégré universitaire de santé et de services sociaux de la Capitale-Nationale : Déficience motrice et douleur chronique
- Centre intégré universitaire de santé et de services sociaux de l’Est-de-l’Île-de-Montréal : Centre de gestion de la douleur
- Centre intégré universitaire de santé et de services sociaux du Centre-Ouest-de-l’Île-de-Montréal : Programmes Autogestion de la douleur chronique, Neurologie, Neuro-musculo-squelettique, Rhumatologie, Traumatisme craniocérébral (TCC) ; Program autogestion de la douleur chronique
- Centre intégré universitaire de santé et de services sociaux du Centre-Sud-de-l’Île-de-Montréal : Clinique d’adaptation à la douleur chronique (18 ans et plus)
- Centre intégré universitaire de santé et de services sociaux du Centre-Sud-de-l’Île-de-Montréal : Clinic de gestion de la douleur chronique (65 ans et plus)
- Centre intégré de santé et de services sociaux de l’Outaouais : Clinique médicale antidouleur Outaouais
- Centre intégré de santé et des services sociaux de l’Abitibi-Témiscamingue : Clinique de gestion de la douleur
- Centre intégré de santé et des services sociaux de l’Abitibi-Témiscamingue : Vivre en santé avec une maladie chronique – a six-week program to help you better self-manage your condition
- Centre intégré de santé et de services sociaux de la Côte-Nord : Douleur chronique
- Centre intégré de santé et de services sociaux de la Gaspésie : Les programmes des maladies chroniques
- Centre intégré de santé et de services sociaux de Laval : Programme d’adaptation à la douleur chronique
- Centre intégré de santé et de services sociaux de Lanaudière : Clinique de la gestion de la douleur
- Centre intégré de santé et de services sociaux de la Montérégie-Centre : Clinique de gestion de la douleur
- Centre intégré de santé et de services sociaux de la Montérégie-Est : Service consultatif de gestion de la douleur – Hôpital Pierre-Boucher
- Nunavik Regional Board of Health and Social Services: Prevention and Health Promotion/ ᖃᓄᐃᖕᖏᓯᐊᕐᓂᒨᓕᖓᔪᓂᒃ ᐃᑯᓪᓚᑎᑦᓯᒐᓱᐊᕈᑏᑦ ᖃᐅᔨᒪᔭᐅᑎᑦᓯᒍ
- Nunavik Regional Board of Health and Social Services: Physical Health/ ᑎᒥᒃᑯᑦ ᖃᓄᐃᖕᖏᓯᐊᕆᐊᖃᕐᓂᖅ
- Nunavik Regional Board of Health and Social Services: Active Lifestyles/ ᐃᙯᓕᓴᖃᑦᑕᓱᓂ ᐃᓅᓂᖅ
- Nunavik Regional Board of Health and Social Services: Healthy Eating/ ᖃᓄᐃᖏᓯᐊᕐᓂᑯᑦ ᓂᕆᓂᖅ
Province-wide
- Nova Scotia Health: Chronic Pain Self-Management Programs
- Nova Scotia Health: Hip & Knee Arthritis Conservative Management Program
- Nova Scotia Health: Wellness Group Programs – including Understanding Pain, as well as many other programs that can help with arthritis symptom management, such as multi-week exercise programs, healthy eating, and meditation
- Nova Scotia Health: Chronic Pain Services (a referral from your doctor is required)
- Nova Scotia Health: Pain Self-Management Patient Resources
- Action Atlantic: information and resources for people with chronic pain
Regional
- Tajikeimɨk Mi’kmaw Health and Wellness
- Millbrook First Nation: Millbrook Health Centre – programs and services for members of Millbrook First Nation
- Sipekne’katik First Nation (Indian Brook): Sipekne’katik Health & Wellness Centre
- Paqtnkek Mi’kmaw Nation: Paqtnkek Health Centre
- We’koqma’q First Nation: We’koqma’q Health & Wellness Department
- Membertou First Nation: Membertou Health & Wellness Home
- Pictou Landing First Nation: Health Department
- Union of Nova Scotia Mi’kmaq: Health Programs and Departments
Province-wide
- Horizon Health Network: Arthritis Clinic
- Union of New Brunswick Indians: First Nation Health Centres
- Vitalité Health Network: First Nations Services
*Please note: Very limited information about pain management or chronic disease management programs and services in New Brunswick was available online at the time of writing. You may wish to visit the following websites to check back for new information:
Regional
- Clinique de douleur de l’hotel dieu du CHUGLD, Medical Director : Dr. Richard Dumais 330 Université Moncton NB E1C 2Z3 Tel : (506) 862-4721
- Pain Clinic at the Campbellton Regional Hospital, Medical Director: Dr. Hristo Laevski 189 Lily Lake Rd, Campbellton NB E3N 3K2 Tel: (506) 789-5000
Province-wide
- Get Better Together – online and in-person programs to support self-management of ongoing health conditions such as arthritis
- Ongomiizwin – Health Services (OHS): Health Programs – health services for Indigenous communities across Manitoba and Nunavut
- Manitoba Métis Federation: Health and Wellness Department – information for Métis people in Manitoba about the MMF’s health initiatives
Regional
- Winnipeg Regional Health Authority: Chronic Pain Self-Management – a series of 7 education sessions to help you cope with chronic pain
- Winnipeg Regional Health Authority: Pan Am Pain Management Clinic (requires a referral from your doctor)
- Winnipeg Regional Health Authority: Chronic Pain Services (requires a referral from your doctor)
- Winnipeg Regional Health Authority: Indigenous Health Resources for Patients
- Interlake-Eastern Regional Health Authority: Free Online Classes for Healthy Living
- Interlake-Eastern Regional Health Authority: Physical Activity
- Interlake-Eastern Regional Health Authority: Wellness Support Line – free telephone support service
- Southern Health: Living with a Chronic Disease Program
- Prairie Mountain Health: Get Better Together
Province-wide
- Pain BC: includes a Coaching for Health program (requires referral from healthcare practitioner), Live Plan Be online pain self-management tool and more
- Self-Management BC: Chronic Pain Toolkit for Active Living – you can participate in this program through self-directed learning online, through a telephone group over six weeks, or through a six-week virtual group. In-person options may also be available, please check website. For Chinese, Indigenous and Punjabi programs, please contact the program coordinators directly.
- Self-Management BC: Better Choices, Better Health® Online Program
- Self-Management BC: Peer Health Coach Program
- OASIS – OsteoArthritis Service Integration System: Our Classes – offers free online classes on osteoarthritis self-management. Information is also available in Punjabi, Farsi, Traditional Chinese and Simplified Chinese.
- First Nations Health Authority: Wellness Streams for First Nations communities. Find tips, guides and resources on Being Active, Eating Healthy, Nurturing Spirit, and Respecting Tobacco.
- Métis Nation of British Columbia: Health and Wellness Newsletter. Information about upcoming health programs and events for Métis people in British Columbia.
Regional
- Vancouver Coastal Health: Mary Pack Arthritis Program – provides information, online educational workshops and services in communities across BC to help you better manage your arthritis. Services may require a referral from your doctor.
- Vancouver Island – Island Health: Pain Management Services
Province-wide
- Health PEI: Patient Navigator Service – this free service can help you navigate the PEI healthcare system to find services, supports and information in your community
- Health PEI: Passport to Health booklet – tips and tools for healthy living
- Native Council of PEI: The PEI Helping Tree – useful resources of community-based services
- Mi’kmaq Confederacy of PEI: Health Programs
*Please note: Very limited information about pain management or chronic disease management programs and services in PEI was available online at the time of writing. You may wish to visit the following websites to check back for new information:
Province-wide
- Saskatchewan Health Authority: LiveWell with Chronic Pain – six week program to support pain self-management
- Saskatchewan Health Authority: LiveWell with Chronic Conditions – six week program
- SaskPain: website with information on pain treatment clinics, self-management skills, physical activity supports, medication, drug-free pain management strategies, mental health, and more
- Saskatchewan Health Authority: Chronic or Complex Pain Management
- Saskatchewan Health Authority: Pain Management Overview
- Saskatchewan Health Authority: Chronic Pain Pathway for Patients
- Saskatchewan Health Authority: First Nations and Métis Health
- Online Therapy Unit: Chronic Health Conditions Course including Chronic Pain – a free 5-lesson cognitive behavioural therapy program to help individuals manage their symptoms
- University of Saskatchewan: Chronic Pain Toolkit – includes information about programs in Saskatchewan, self-management strategies and more
- Métis Nation of Saskatchewan: Health and Well-Being – health and wellness news for Métis people in Saskatchewan
Regional
- Saskatoon: LiveWell Rheumatology Program – for people with arthritis and rheumatic illnesses
- Saskatchewan Health Authority: Chronic Disease Management Programs (programs and services offered outside of Saskatoon)
Province-wide
- Alberta Health Services : Better Choices, Better Health® Chronic Pain Management Program – a free six-week program currently being offered online
- Alberta Health Services: Alberta Healthy Living Program
- Alberta Health Services: Rehabilitation Advice Line or 1-833-379-0563 – free telephone service that provides rehabilitation advice and general health information to Albertans
- Alberta Health Services: Chronic Pain Management Lecture Series – a video series to help viewers understand and better self-manage pain
- Pain Society of Alberta: Resources for those who Live with Pain
- Métis Nation of Alberta: Health Programs – culturally appropriate, self-directed health programs for Métis Albertans
Regional
- Calgary: Calgary Chronic Pain Program (some services may require a referral from your doctor)
- Calgary Foothills Primary Care Network: Chronic Pain Management Program (requires a referral from your doctor)
Province-wide
- Government of Newfoundland and Labrador: Improving Health: My Way chronic disease self-management program
- First Nations of Quebec and Labrador Health and Social Services Commission: Health and Wellness Services – information about programs and services for First Nations communities in Labrador
Regional
- Eastern Health: Centre for Pain and Disability Management – five-week self-management program (requires a referral from your doctor)
- Eastern Health: Chronic Pain and Disability Management Resources
- Western Health: Improving Health: My Way chronic disease self-management program
- Central Health: Improving Health: My Way chronic disease self-management program
- Central Health: Health Coach Program – free program to help you manage your health
- Labrador-Grenfell Health: Improving Health: My Way chronic disease self-management program
- Nunatsiavut Government: Health Services
- Nunatsiavut Government: Department of Health and Social Development
Territory-wide
- Government of Yukon: Your Health, Your Way program – free 6-week chronic disease self-management program
- Yukon Health Guide: Community Support
- Yukon Health Guide: Community Hospitals and Health Centres
- Yukon Health Guide: Community Hospitals and Health Centres – First Nations Services
- Government of Yukon: Register for a free exercise program for people with chronic conditions
- Government of Yukon: Relaxation Techniques Brochure
Regional
First Nations Departments of Health: *Please note, for medical services in First Nations communities, please visit Community Hospitals and Health Centres – First Nations Services
- Carcross/Tagish First Nation: Department of Health and Wellness
- Champagne and Aishihik First Nations: Community Wellness
- First Nation of Na-Cho Nyäk Dun: Health and Social
- Kluane First Nation: Wellness and Education
- Kwanlin Dün First Nation: Health Services
- Liard First Nation: Health Services
- Little Salmon/Carmacks First Nation: Health and Social
- Ross River Dena Council: Community Programs and Services
- Selkirk First Nation: Health and Social Programs
- Ta’an Kwäch’än Council: Health Department
- Tr’ondëk Hwëch’in: Wellness
- Teslin Tlingit Council: Health and Social
- Vuntut Gwitchin First Nation: Health and Social Programs
- White River First Nation: Wellness
Territory-wide
- Northwest Territories Health and Social Services: System Navigator – call toll-free for help and information about accessing services 1-855-846-9601
- Government of Northwest Territories: Chronic Disease Resources
- Northwest Territories Health and Social Service Authority: Nutritional Food Fact Sheets
Regional
- Northwest Territories Health and Social Services Authority: Stanton Rehabilitation Persistent Pain Program – free 6-part pain management program open to the NWT Yellowknife Health Region (including Behchokǫ̀, Łutsel Kʼe, Whati, Nahanni Butte, Fort Simpson, Jean Marie River, Fort Providence, Ndilǫ, Fort Liard, Gameti, Wekweètì, and Wrigley) and the Kitikmeot Region of Nunavut
- Tthets’éhk’ehdélį – Jean Marie River First Nation: Health and Wellness Programs and Services
- Gwich’in Tribal Council: Health & Wellness
- Acho Dene Koe First Nation: Community Wellness Workshops and Services
- Inuvialuit Regional Corporation: Health and Wellness
Territory-wide
- Free Rehabilitation Services, including physiotherapy and occupational therapy: Rehabilitation Services/ Mamittirpallianikkut/ ᐊᑲᐅᓯᓴᖅᑕᐅᓂᖅ
- Inuusittiaringniq Living well together: Chronic Diseases Information/ Aaniarutiryuaq aanniarut/ ᐱᔪᓐᓂᕈᓐᓇᙱᑦᑐᒥᒃ ᐊᓐᓂᐊᖃᕐᓂᖅ
- Inuusittiaringniq Living well together: Active Living/ Huliluqaaraanginnaqhuni Inuuhiq/ ᐃᖃᐃᓕᓴᖃᑦᑕᕐᓂᖅ
- Inuusittiaringniq Living well together: Healthy Eating/ Niqigiktunik Niriniq/ ᓂᕿᑦᑎᐊᕙᓐᓂᑦ ᓂᕆᓂᖅ
- Government of Nunavut: Health Centres Map/ Munarhiliqiviuyut Naunaitkut/ ᐋᓐᓂᐊᖅᑐᓕᕆᓂᕐᒧᑦ ᐃᓂᒋᔭᐅᔪᑦ ᓄᓇᙳᐊᖓ
- Ongomiizwin – Health Services (OHS): Health Programs – health services for Indigenous communities across Nunavut and Manitoba
Regional
- Stanton Rehabilitation Persistent Pain Program – free 6-part pain management program open to the the Kitikmeot Region of Nunavut and the NWT Yellowknife Health Region
Online Guides to Chronic Pain Management
This section includes links to online guides to help you learn about pain management on your own time. Each guide includes mini lessons or resources to prepare you with the knowledge needed to better manage your own or your child’s pain.
Thank you to Oneida Baxhia for her contributions to this project.
This resource was made possible through educational grants from:
 |
 |
 |

 Chronic pain can have an impact on our mental health just as our mental health can impact the way we experience pain. For more information to help you take care of your mental health, visit the
Chronic pain can have an impact on our mental health just as our mental health can impact the way we experience pain. For more information to help you take care of your mental health, visit the 