Pain is a fact of life for many people with arthritis, and that can be a scary or frustrating thought. Thinking it’s out of your control and trying to ignore it is a common response, and while that’s an understandable human reaction, it’s not the best approach. The secret to managing pain is to be strategic and pay attention to various factors going on in your life. It means understanding the pain cycle. Let’s take a closer look at what the pain cycle is and how to disrupt it so you can take more control of your symptoms.
The pain cycle
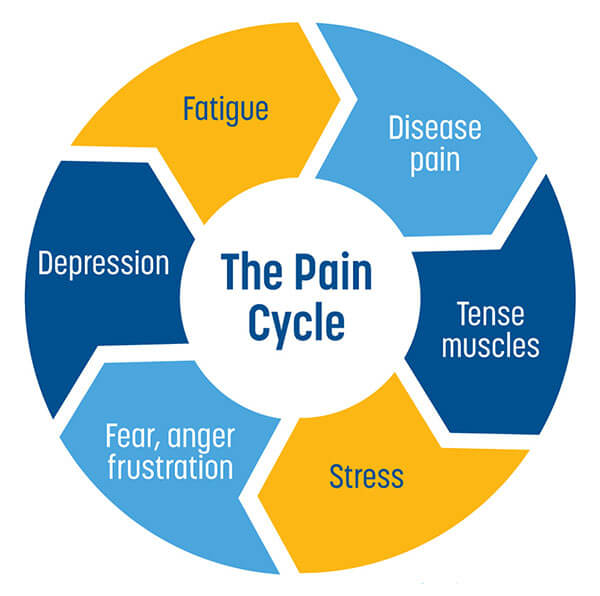
Persistent or chronic pain is affected by five main factors that can impact each other:
- Physical problems caused by injury, disease or surgery
- Tense muscles (which may actually be your body’s reaction to protect injured joints)
- Psychological stress
- Depression or other negative emotions and feelings
- Fatigue
An increase or decrease in any of the factors can affect how you experience pain. If you think about it, you can probably pinpoint situations when your pain seems to get better or worse. When you’re laughing over a card game with friends, you don’t notice your pain as much. If you’re lying awake worrying over the news headlines, your pain levels can spike.
You might also notice times when these factors interact with each other, resulting in increased pain. You might have tight muscles because you’re reacting to pain—the muscles are bracing around your sore joint. However, tight muscles can also cause pain, because your activities are stressing the tense muscles.
Another cause of tight muscles is stress. When you’re feeling stressed, your muscle tension can increase, which in turn can make pain feel worse. Stress can also lead to feelings of anger, frustration and fear. These negative emotions are mentally and physically tough to deal with, and lead to exhaustion and fatigue. Because these factors can worsen pain as well, finding ways to help manage your stress can also help you manage your pain.
The pain cycle goes both ways: while feeling down or depressed can contribute to your pain, feeling in pain may also cause you to stop doing things you enjoy, such as cancelling social activities with your friends, which can in turn lead to feeling down or isolated.
In addition to emotional factors that can contribute to the experience of pain, there’s also a chemical component to consider. Our body produces natural chemicals when we are stressed, tired, anxious or depressed. These chemicals are very close to chemicals the body uses to signal damage or danger. So, if you’ve had persistent pain over time, the chemicals triggered by low moods can actually amplify feelings of pain. Some experts refer to this as “turning up the volume” of pain. In other words, the body’s nervous system gets sensitized and overreacts.
So, pain isn’t always straightforward. However, understanding what’s going on can go a long way to “turning down the volume” on pain. Here’s what to keep in mind.
Breaking the pain cycle
Stress, fatigue and depression are closely related to pain. By paying attention to how these elements affect your pain levels, you can also take steps to reverse or interrupt the cycle.
Your brain sends different signals to your body that can affect the way you experience pain. These signals can trigger chemicals that help suppress pain messages to the body. To boost the release of these chemicals, you can try physical activity and relaxation or visualization techniques. After reading an article about the pain cycle two years ago, Jennifer Boyle of Toronto has found success with a variety of techniques. “I follow my treatment plan and take my medication, but I also try to be creative. When my legs hurt, I pretend I’m lying on a beach in the sun and that helps to relax the muscles,” says Jennifer, who has been living with psoriatic arthritis for 26 years. If she’s out for a walk and every step hurts, instead of focussing on the pain, she tries to distract herself by paying attention to something else in her environment, like trees or flowers.
Like many people living with arthritis, Jennifer has difficult days when her condition makes her feel fed up, angry or scared. “I find if I label what I’m experiencing, it helps: ‘I am tired because of this situation. I am stressed out because my knee hurts.’ Take a step back and say, ‘ok, this is part of the disease, and I’m going to do the best I can to manage it.” Self-management is the key, she adds. “It took me a long time for me to realize you have to become a manager of your disease. You just can’t let it passively take over your life. You have to try to work on your stress levels, work on your emotions and try everything that’s possible to manage it.”