Information, resources and tools to help you manage your gout symptoms and improve function.
Gout is the most common form of inflammatory arthritis, affecting as many as 1 million Canadians.
Gout can happen when there is too much uric acid in the bloodstream. Uric acid is produced by the breakdown of purines, which are found in the foods we eat.
Kidneys help to filter out uric acid, which our bodies get rid of through urine. When the kidneys are not able to filter or process uric acid levels at the same rate they are being created, this can cause high uric acid levels to remain in the bloodstream.
Genetics play an important role for those at risk of having gout. Some bodies will breakdown purines into uric acid and be able to excrete excess uric acid more easily than others. Even if two people have the exact same diet and eating habits, one person could have higher levels of uric acid in their bloodstream, and be at an increased risk of developing gout.
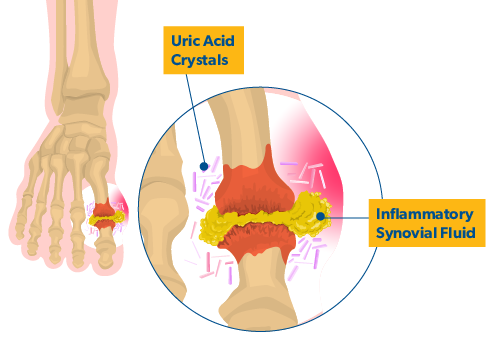
After months to years of sustained high level of uric acid in the bloodstream (usually above 400 µmol/l) the uric acid can leave the bloodstream and form uric acid crystals in joints and soft tissues.
Uric acid crystals in soft tissues are usually found under the skin and form hard bumps with a white chalk-like colour. When they are present, these crystal deposits, called tophi [toe-fi] can usually be seen around the ears and around extensor tendons, which are found in hands and feet. Uric acid crystals in joints can be responsible for gout attacks.
FAQs
What are risk factors for gout?
 Since gout is directly related to uric acid levels in the blood, these risk factors are primarily associated with the production and excretion of uric acid:
Since gout is directly related to uric acid levels in the blood, these risk factors are primarily associated with the production and excretion of uric acid:
- Diet: Foods such as red meat, certain seafoods (i.e., shrimp and oily fish), alcoholic beverages (especially beer), sugar, and fructose (often found in soft drinks) can all increase uric acid levels.
- High blood pressure: High blood pressure and some medications used to treat high blood pressure (diuretics) increase the risk of gout. Taking low dose aspirin also increases uric acid levels.
- Obesity: People with high body weight are more likely to develop gout and at a younger age than those with lower body weight. Over the past twenty years, the incidence of gout has nearly doubled, likely connected to an increase in obesity in the general population.
- Medication: Some medications block the excretion of uric acid in the kidney. In general, diuretics and certain medications that suppress the immune system can increase risk of gout.
- Trauma: Gout can be brought on by surgery, heart attack, or other physical and even emotional trauma.
- Kidney disease: Even mild kidney disease can result in reduced excretion of uric acid from the body.
- Heredity: If someone in your family has gout, you have a higher chance of developing the disease since gout does run in some families. However, many people who develop gout do not have a family history of the disease.
- Dehydration: Dehydration can contribute to gout attacks.
How common is gout?
As many as 1 million Canadians are estimated to have gout, about 2-4% of the population. Gout is the most common form of inflammatory arthritis and affects more males than females (about 4% vs. 1%). The number of people who have gout has been increasing globally over time, as well as the number of new diagnoses. Gout is more common as people get older.
While these gout statistics likely reflect a primarily cisgender population, limited research indicates that the use of long-term hormone therapy by trans people is associated with changes in uric acid levels, which could have implications on gout development. Further research is needed.
If you have concerns about a possible change in uric acid levels due to hormone use or have other conditions that may increase your risk of gout, consult with your doctor about how to best monitor your risk.
What happens during a gout attack?
 Gout attacks can only happen if there are uric acid crystals within the joint, which only occurs if there is too much uric acid in the bloodstream.
Gout attacks can only happen if there are uric acid crystals within the joint, which only occurs if there is too much uric acid in the bloodstream.
Once the crystals are inside the joint, the immune system will sometimes try to get rid of the crystals. Under certain circumstances, white blood cells, which are part of our immune system, can migrate from the bloodstream into the joint where the uric acid crystals are present. Those white blood cells, called neutrophils, will try to destroy the uric acid crystals. In the hope of getting rid of the crystals, the neutrophils will multiply within the joint, which leads to inflammation, swelling, redness and pain in the affected joint. This is known as a gout attack.
The neutrophils are not strong enough to eliminate the uric acid crystals in the joint, and after a couple of days they will die off, and the gout attack will be over. However, the uric acid crystals within the joint will remain, leaving the person at high risk of subsequent gout attacks if measures are not taken to reduce them.
Symptoms and Diagnosis
What are early signs and symptoms of gout?
 Gout attacks, particularly early ones, may appear to come on suddenly, but this is often the result of months or even years of uric acid levels building up in the bloodstream. After a long period of sustained high uric acid levels, it can begin to leave the bloodstream and start forming crystals in the joints and soft tissues.
Gout attacks, particularly early ones, may appear to come on suddenly, but this is often the result of months or even years of uric acid levels building up in the bloodstream. After a long period of sustained high uric acid levels, it can begin to leave the bloodstream and start forming crystals in the joints and soft tissues.
Gout attacks are often triggered by the body’s immune system responding to the uric acid crystals that have formed in the joints and soft tissue. When immune cells called neutrophils enter the joint to try and eliminate the uric acid crystal, this is when inflammation, redness, pain, and swelling will appear, causing what is known as a gout attack.
Uric acid crystals can build up in multiple joints, but gout attacks are more common in lower limb joints such as the knees, ankles, and particularly the base of the big toe.
Many people will not have any indication they have gout before a first gout attack.
As we go about our daily lives, micro-traumas can occur in our body and joints which may cause neutrophils to rush to those areas to help with the healing process. If your joint already has a buildup of uric acid crystals, this rush of neutrophils sent as part of the regular healing process may also detect the uric acid crystals and start responding to try and get rid of them. This process could trigger a gout attack. Since these micro-traumas are often more common in lower limbs and joints, these areas are more common sites for a gout attack.
Other risk factors for a gout attack are infection, a drastic increase in uric acid levels in the bloodstream — for example following a protein-rich meal, a night of drinking alcohol (especially beer), or a period of dehydration.
What are tophi?
Bumps can form when uric acid crystals build up under the skin. These bumps, called tophi, are usually small and hard and can form anywhere on the body. Often they form on the toes, knees, heels, fingers, ears, forearms or elbows. Tophi are usually painless; however, sometimes they can become inflamed and ooze a thick discharge. Tophi often form several years after the first gout attack and in some cases they appear in people who have never had a gout attack.
How is gout diagnosed?
 To diagnose gout, your doctor will ask about recent medications and diet. They will want to know:
To diagnose gout, your doctor will ask about recent medications and diet. They will want to know:
- when symptoms began
- how long symptoms or attacks last
- the intensity of your symptoms or attacks
- which joints are involved or affected by symptoms
A blood test can determine uric acid levels, but high levels do not necessarily indicate a gout attack. During an active attack, your doctor may send you for blood work to check your uric acid levels. They may ask you to repeat a blood test after your attack has ended, to compare your uric acid levels during and after an attack.
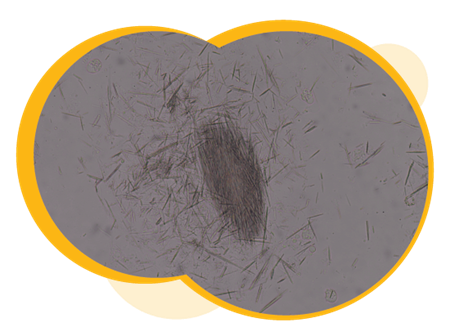
To receive a confirmed diagnosis of gout, your doctor will need to take a fluid sample from your joint during a gout attack. To do this, they will insert a needle into the affected joint and extract a sample.
The sample will then be examined under a microscope to determine if neutrophils are actively trying to destroy the uric acid crystals. If this activity is observed in the fluid sample, your doctor will be able to confirm a gout diagnosis. When neutrophils try to destroy the crystals, the crystals are described as being intracellular.
Although taking a fluid sample is the most definitive way of diagnosing gout, this is not always possible or necessary depending on your situation. Your doctor can also make a presumed diagnosis based on a combination of signs, symptoms, and test results, such as blood work, x-ray, and ultrasound.
Treatment
Why is treatment for gout so important?
Gout attacks tend to increase in length and frequency without treatment and can even become chronic. The ongoing presence of uric acid crystals in and around the joint can lead to destruction of the joint and the soft tissues around it.
Fortunately, with proper medical attention and treatment, few patients progress to this advanced stage. Most people living with chronic gout can control the condition with medication. Lifestyle changes are an important part of treatment and can help prevent and manage flares. Early identification and treatment can reduce the chance of permanent joint damage and the number and severity of attacks.
How is gout treated?
Treatment for gout consists of three main steps:
Step 1: Treat active gout attack.
Step 2: Lower uric acid levels in the bloodstream (if indicated).
Step 3: Add a prophylactic treatment if a medication is given to lower the uric acid in the bloodstream.
When having an attack

When having a gout attack, take these steps to bring pain and swelling under control:
- Ice, elevate and rest the joint.
- Take colchicine, anti-inflammatory medication, or prednisone as soon as possible, as advised by your doctor.
- Drink plenty of water and fluids. Remember alcohol, pop, or sugary drinks can trigger gout attacks, so avoid those.
- Keep track of which joints are involved, the intensity and any changes in pain, and the length of the attack.
- Call your doctor to make an appointment to be assessed.
- Avoid stress as much as possible. Added stress can make a gout attack feel more intense. Consider using relaxation techniques such as mindfulness meditation to relax your body’s response to pain.
Heat and cold
 Cold
Cold
During a gout attack, using cold can help reduce pain. Cold reduces blood flow to the injury, which helps reduce swelling and inflammation. Cold should not be applied for longer than 20 minutes at a time. As a general rule, 20 minutes on, 20 minutes off, works well. Always use a protective barrier, such as a towel, between any cold pack and the skin.
Using a commercial cold pack or a homemade one (from crushed ice, ice cubes or a bag of frozen vegetables) can be helpful.
Cold is ideal for:
- Swelling
- Decreasing pain
- Constricting blood flow to an inflamed joint
 Heat
Heat
Heat should not be used during a gout attack since applying heat can make symptoms worse. However, between attacks, taking a warm shower and using warm packs (such as hot water bottles or microwavable heating pads) are great ways to help reduce general pain and stiffness.
Heat is ideal for:
- relieving pain and stiffness
- relieving muscle spasms and tightness
- enhancing range of motion
IMPORTANT: Do not use heat on an already inflamed joint, as it can make symptoms worse.
flourish articles:
- Cold therapy for arthritis: Learn how cold therapy can help manage joint pain, swelling and inflammation.
- Heat therapy for arthritis: Heat therapy can help decrease pain by relaxing muscles and increasing circulation.
Relaxation techniques and skills

Developing good relaxation skills can help you maintain balance in your life, giving you a greater feeling of control over your gout and a more positive outlook. Relaxing the muscles around a sore joint can help to reduce pain, though it is not always easy to relax when feeling pain. Gout attacks tend to be very painful, but there are techniques you can learn to help you refocus your mind, and help relax your muscles during a painful attack.
Visualization techniques, such as imagining burning sensations being put out by cold water, or concentrating on imagining what your pain might look like can also help to draw focus away from the pain itself, and help you reframe your experiences of pain or discomfort.
Other techniques to consider include mindfulness meditation, deep breathing exercises, listening to a podcast or audio book, narrated relaxation exercises, or soothing music.
A key to developing relaxation skills is to also practice the techniques that feel most comfortable for you even when you are not experiencing pain. This can be especially helpful for forms of meditation and visualization.
Complementary information:
- Meditation for Arthritis: Find information to help you understand more about this therapy, if it can help with your symptoms, and how to find a provider.
Medications to treat an acute gout attack
A number of medications do a good job of preventing pain and swelling in the short-term. Depending on the severity of the gout attack, medications can be given individually, or in combination.
- Non-steroidal anti-Inflammatory drugs (NSAIDs)
- Non-steroidal anti-inflammatory drugs (NSAIDs) are used to treat pain and inflammation. The term “non-steroidal” means that they do not contain steroids. NSAIDs are commonly used drugs, and there are many different types and brands. Many can be obtained without a prescription. These medications control the symptoms of gout, but do not alter the course of the disease. NSAIDs can be taken as needed or taken regularly to control symptoms. While generally well tolerated, NSAIDs may irritate the stomach or cause other side effects. Talk with your doctor to decide if NSAIDs are an appropriate treatment option for you.
- Colchicine
- For those unable to take NSAIDs, colchicine is an option that has been used to treat gout for more than 2,000 years. Originally from a plant extract, colchicine is often used to relieve the pain and swelling of gout attacks. By intervening in this early phase of a gout attack, colchicine can reduce the production of neutrophils that cause pain, inflammation, and swelling. When taken after the first 48 hours of an attack, the neutrophils have often had too much time to enter the affected joint, and colchicine will provide little to no benefit.While effective, many people cannot take colchicine due to its side effects; however, you and your doctor can decide if colchicine is right for you.
- Corticosteroids
- For those who cannot take NSAIDs or colchicine, corticosteroids may be a good alternative. These are given either orally or as injections into the affected joints. Injections tend to work quickly – within a few days or even within a few hours for some people. If you would like to explore this option, discuss with your doctor to determine if corticosteroids make sense for your treatment plan.
Lowering uric acid in the bloodstream
After a first gout attack, your doctor will discuss with you whether you may benefit from medications to help lower the level of uric acid in your bloodstream. Your doctor will consider the following indications to help make this decision:
- Two or more gout attacks within the span of 12 months
- A history of kidney stones
- Chronic kidney failure
- Bone erosion on x-ray
- Presence of tophi (uric acid crystals under the skin – pronounced toe-fi)
When working with you to lower your bloodstream uric acid levels, your doctor will want to help you reach the following target uric acid levels in your bloodstream.
- If you have no erosion or tophi present, uric acid levels should be less than 360 µmol/l.
- If there is erosion or tophi present, uric acid levels should be below 300 µmol/l
Medications that reduce uric acid levels
 To achieve lower bloodstream levels of uric acid, your doctor may prescribe a medication. Medications that reduce uric acid levels will prevent future gout attacks and keep the condition from becoming chronic.
To achieve lower bloodstream levels of uric acid, your doctor may prescribe a medication. Medications that reduce uric acid levels will prevent future gout attacks and keep the condition from becoming chronic.
Taking medications that regulate uric acid levels is often a long-term treatment option since starting and stopping these medications can trigger a gout attack. Your doctor may wait to introduce this type of medication to first determine how frequently you experience gout attacks, and if they can be controlled through other treatment options. If you experience two to three attacks per year, your doctor may wish to explore this medication option with you.
Since starting a medication to lower uric acid levels can also trigger a gout attack, your doctor will likely also prescribe another medication, usually an NSAID or colchicine, to take daily for the first few months to help prevent further gout attacks while your body adjusts to taking a uric acid lowering medication.
Once you start a medication to lower uric acid levels, you may not notice any benefit right away. In some cases it could take years to achieve target uric acid levels, and for the uric acid crystals in joints and soft tissues to disappear.
The following medications are commonly used to help lower uric acid levels in the bloodstream:
- Allopurinol
- Allopurinol is a medication used to lower uric acid levels. It can take several weeks for the effects to become noticeable. It is common for a gout attack to happen in the first few months after starting allopurinol. Continue to keep your doctor informed of any new symptoms you may experience. If you have concerns about any side effects, or still have gout attacks while taking allopurinol, talk with your doctor about your treatment plan. Allopurinol may interact with other medications you are already taking. You and our doctor can decide if taking allopurinol is right for you.
- Febuxostat
- Febuxostat works to reduce the level of uric acid in the body, which can help in the management of gout. Although febuxostat is generally well tolerated, it is always best to have a conversation with your doctor to decide if febuxostat is right for you and your treatment plan.
- Pegloticase
- If other medications are not effective at lowering uric acid levels, pegloticase may be used as an alternate option. Pegloticase may only be used if no other treatment options have been found effective. Many people experience side effects that make them unable to tolerate this medication. Talk with your doctor to determine if pegloticase is right for you. This medication should not be used in people with a history of kidney stones.
For more information about medications, consult our Medication Reference Guide.
Surgery
Surgery is rarely required for gout. Occasionally, surgery is considered for people who have suffered from gout over a long period of time to remove problematic tophi or to repair badly damaged joints. However, with proper medication and treatment, these situations are generally avoided.
Self-Management
Given the direct link of gout to uric acid levels, managing it depends primarily on a strategy for eating well and managing the intake of foods that contribute to increased uric acid levels. Healthy kidney function is important as well, since uric acid is removed from the blood by the kidneys. The kidneys rely on the heart to efficiently pump the blood through the body. People who are overweight are more prone to heart disease, so staying physically active and managing weight can help in controlling gout.
Food choices
When the body processes purines from foods and other sources, uric acid is a byproduct. One way to help reduce the level of uric acid being produced by the body is to reduce the level of purine intake through food.
Managing gout includes monitoring the type of foods and beverages you are consuming, making sure to avoid food or drinks that are high in purines that can cause a build-up of uric acid and trigger a gout attack.
In general, those suffering from gout should AVOID the following foods:
- processed meat
- red meat and organ meats (such as liver, tongue and sweetbreads)
- shellfish (such as shrimp, lobster and mussels)
- oily fish (such as herring, sardines and mackerel)
- sugary beverages (including pop and some juice)
- any food, drinks or sauces that contain corn syrup
- excessive alcohol (Any amount of alcohol affects uric acid production and disposal, but more than one drink in a day for women and more than two drinks in a day for men is especially dangerous. Beer, in particular, has been linked to gout attacks.)
Consult with a registered dietician to learn more about what food and diet adjustments make sense for your needs. Some people have found the following foods to be helpful in managing their gout, however, each person’s experience will vary.
- skim milk and other low-fat dairy products
- cherries and citrus fruits
- vitamin C supplements (500–1,000 milligrams daily)
- coffee
If you are considering adding vitamins or supplements to your diet, it is recommended to first discuss with your treating doctor.
While diets high in meat and fats are more commonly known to trigger gout attacks, vegan and vegetarian diets can also trigger a gout attack depending on what type of foods are being consumed. If you already avoid all of the recommended foods listed above but are still struggling with gout attacks, talk with your doctor, and ask to speak to a dietitian who can help you find meal plan options that work for you.
Complementary information:
- Recipes on flourish
- Gout and nutrition: Learn about how food and drink choices can help prevent and treat gout, including information about alcohol, protein and the DASH diet.
- Understanding arthritis and alcohol: Understanding how alcohol affects arthritis, including medication interaction, managing weight, sleep, gout and mental health.
Eating well to control weight
 Gout is more common in people who are overweight. Losing weight and maintaining a healthy body weight can help manage gout. Losing weight reduces uric acid levels in the blood – and for many people, the more weight they lose, the more their uric acid levels decrease. Maintaining a healthy weight also decreases the risk of heart disease, which has been shown to contribute to gout symptoms.
Gout is more common in people who are overweight. Losing weight and maintaining a healthy body weight can help manage gout. Losing weight reduces uric acid levels in the blood – and for many people, the more weight they lose, the more their uric acid levels decrease. Maintaining a healthy weight also decreases the risk of heart disease, which has been shown to contribute to gout symptoms.
Proper nutrition is vital to controlling body weight. Here are three ways to cut back on excess calories:
- Reduce fat intake: A healthy diet should include a small amount of unsaturated fats and limited amounts of saturated and trans fats. Choosing the right amount and types of fats can help you achieve and maintain a healthy body weight.
- Reduce processed and added sugars: Processed and refined sugars add extra calories that can contribute to weight gain. Additional fat tissue from weight gain can also increase an inflammation response.
- Eat more fruits and vegetables: Fruits and vegetables should make up the largest component of your diet. Sugar intake is still a concern when eating fruit, even though it has natural sugars. Consider eating mostly low sugar fruits to reduce your overall sugar intake. Try to have at least one fruit or vegetable at every meal and while snacking. In addition to being an excellent source of energy, fruit and vegetables increase your fibre intake, which can help with weight management. Fruits and vegetables are loaded with antioxidants, which help boost the immune system and may help maintain healthy joints.
Complementary information:
- Understanding nutrition labels on food: Eating Well can play a large role in helping you manage arthritis symptoms, so understanding nutrition labels is important.
- The right exercise mix: Understanding the different kinds of exercise – flexibility, strength and endurance – and how they work together as part of an arthritis physical activity plan.
Try to avoid triggers
Gout is often brought on by external stresses, so being aware of these and avoiding them where possible can assist in preventing further attacks. These are some of the triggers that can bring on gout attacks:
- joint injury
- surgery
- infection
- diuretic medications
- forgetting to take your gout medication
- crash diets and fasting
- drinking too much alcohol
- eating large quantities of foods high in purines dehydration
Arthritis Talks Webinars
Arthritis Talks webinars on the latest guidance direct from arthritis experts to help you get more out of life with gout.
 |
 |
 |
| Understanding Gout | Gout Self Defence: Preventing Painful Attacks | Eat Smart for Arthritis |
| In this Arthritis Talks webinar rheumatologist and gout expert, Dr. Jean-Philip Deslauriers, delves into everything you need to know… | Dr. Alexa Smith discusses gout at a public forum in Saint John presented by The Arthritis Society on November 18th, 2015… | We know eating well can make a big difference when you live with arthritis. But figuring out what works best for you may feel… |
| View More Webinars |
Contributors
This gout resource was reviewed in October 2022 with expert advice from:
Dr. Jean-Philip Deslauriers
Clinical Professor at the University of Sherbrooke
Rheumatologist
Bathurst, New Brunswick

