All movement involves our joints. When living with arthritis, joint symptoms like pain, stiffness and swelling can impact many aspects of daily life. Taking care of joint health, moving properly, and strengthening muscles surrounding the joints are top priorities in any arthritis treatment plan.
Visit the sections below to discover what counts as physical activity, how it can help with arthritis pain, and how to get moving and stay active. There is also a curated list of arthritis-friendly exercise resources that you can re-visit for ideas on how to get started.
Physical Activity Guide
What is physical activity?
 Playing sports, swimming, walking with friends, or even pulling weeds in the garden are all examples of physical activity.
Playing sports, swimming, walking with friends, or even pulling weeds in the garden are all examples of physical activity.
Physical activity includes any time you use your muscles to move your body to spend some energy and raise your heart rate. Exercise is one type of physical activity that includes structured activities like going to the gym, attending an exercise class, heading out for a jog or a wheel. But many of the other things you do in your daily life at home, school, work, or recreational settings are also physical activity.
What type of physical activity do you do each day, or each week? Write out a list and keep track of what keeps you moving – whether it’s doing laundry, mowing the lawn, taking a yoga class, or going for daily walks. It all counts toward movement.
Types of physical activities
A wide variety of movements can be considered physical activity. For example:
 Recreational sports or activities like running, canoeing, swimming, water aerobics, golfing, lacrosse, dancing, skiing, skating, or martial arts
Recreational sports or activities like running, canoeing, swimming, water aerobics, golfing, lacrosse, dancing, skiing, skating, or martial arts- Mind-body activities like yoga or tai chi
- Walking, cycling, or wheeling
- Outdoor activities like gardening, yardwork, or gathering or harvesting foods
- Indoor activities and tasks of daily living like cleaning the house, cooking, and going up and down stairs
- Exercises prescribed by a health and exercise professional
Exercise is a type of planned, structured physical activity that is designed to maintain or improve physical fitness. Activities like lifting weights, walking on a treadmill, or taking a yoga class are different forms of exercise that specifically work to improve strength, endurance, or flexibility.
There are different types of exercise that can work together to support health and wellness:
- Therapeutic exercise: Often developed with the help of a healthcare professional (e.g., a physiotherapist), this is a set of planned motions designed to help you improve a rehabilitation goal. It may incorporate awareness of body posture and alignment. Outcomes include developing ‘muscle memory’ by training your joints and muscles to move in healthy patterns, strengthening your muscles, and improving balance or mobility.
- Range of motion exercise: These are also called stretching or flexibility exercises, and they keep your joints moving to help reduce pain and stiffness. To achieve the most benefit, these exercises are done regularly.
- Strengthening exercise: These maintain or increase muscle tone and protect your joints. Resistance-based exercises include weight-training movements done with free weights, your own body weight, resistance bands or weight machines. The frequency and intensity of strengthening exercises should be discussed with a doctor, physiotherapist, kinesiologist, or other qualified health and exercise professional.
- Endurance exercise: These activities – like walking, swimming, and cycling – help you to keep going for long periods of time. They strengthen your heart, give you energy, help control your weight, and help improve your overall health.
- Mind-body exercise: Activities like tai chi, yoga, pilates or martial arts that combine mental focus, controlled breathing, muscle strengthening, flexibility, and balance exercises can also be meditative, promoting relaxation and wellness.
Physical activity and arthritis
When it hurts to move, your first instinct might be to completely stop. But it’s not that simple. Physical activity is one of the most effective ways to reduce pain and improve mobility for people with arthritis.
You may have heard the saying, “motion is lotion.” Movement and physical activity have many benefits for managing arthritis symptoms, including joint pain.
 How does this work? Part of the answer lies in the cartilage – the flexible connective tissue that protects and cushions the bones in many joints. Cartilage needs to absorb nutrients and eliminate waste from the surrounding joint fluid. As you move your joints, you’re ‘feeding’ them by compressing and expanding the cartilage like a sponge, sending blood flow to the moving areas, helping it get what it needs to stay healthy.
How does this work? Part of the answer lies in the cartilage – the flexible connective tissue that protects and cushions the bones in many joints. Cartilage needs to absorb nutrients and eliminate waste from the surrounding joint fluid. As you move your joints, you’re ‘feeding’ them by compressing and expanding the cartilage like a sponge, sending blood flow to the moving areas, helping it get what it needs to stay healthy.
The less you move your joints, the more stiff and painful they become. The muscles that protect the joints also become weaker, leaving you less able to protect them and more prone to injury. Physical activity supports healthy joints, reducing pain and other symptoms.
Here are just some of the known benefits of physical activity that can make a meaningful difference in the lives of people living with arthritis:
- Less pain and stiffness
- Less fatigue and better sleep
- More strength in joint muscles, cartilage, bone, and ligaments
- Better balance and less risk of falls
- Maintenance of a healthy body weight and decreased risk of many other chronic diseases (e.g., heart disease, stroke, diabetes)
- Improved mood and ability to cope with stress
- Opportunities to be social
When it comes to physical activity for people with arthritis, any movement is better than no movement.
Additional information:
Injuries from activity and arthritis
Exercise and other forms of physical activity can help manage arthritis. You might be wondering, though, whether physical activity can cause arthritis or make it feel worse.
 Sports injuries to joints like the knee can put you at a higher risk of developing osteoarthritis (the most common form of arthritis) later in life. When the injury happens in youth, this can also lead to osteoarthritis at a younger age than is often expected. This can be due to joint damage as well as weight gain resulting from lower activity levels after injury.
Sports injuries to joints like the knee can put you at a higher risk of developing osteoarthritis (the most common form of arthritis) later in life. When the injury happens in youth, this can also lead to osteoarthritis at a younger age than is often expected. This can be due to joint damage as well as weight gain resulting from lower activity levels after injury.
With any type of new physical activity, some discomfort or soreness can be normal and doesn’t mean that activity is damaging your joints. Many people with arthritis also become accustomed to living with some degree of pain. Listen to your body and consider whether any pain you experience during or after physical activity is usual or unusual for you. If your joints hurt more than usual and it takes more than two hours to settle down to usual pain levels after being active, you might need to modify that activity. Increasing your activity level gradually and pacing it with how you’re feeling is also recommended.
Before starting a new physical activity or exercise routine, we recommend consulting with your healthcare team or a specialized professional like a physiotherapist to make sure you’re protecting your joints, modifying activities optimally, working with any past or new injuries, and on the path to more mobility and less pain.
How much physical activity do I need?
 Several health organizations have considered available evidence and experiences to create formal recommendations for a healthy level of physical activity. These targets may be challenging to meet at times, especially for those with an episodic chronic disease like arthritis. But working towards any of these goals can have beneficial impacts on your health, and consulting with your healthcare team can help you come up with the best goals for your specific situation.
Several health organizations have considered available evidence and experiences to create formal recommendations for a healthy level of physical activity. These targets may be challenging to meet at times, especially for those with an episodic chronic disease like arthritis. But working towards any of these goals can have beneficial impacts on your health, and consulting with your healthcare team can help you come up with the best goals for your specific situation.
In 2020, the World Health Organization (WHO) released guidelines on physical health and sedentary behaviour (like sitting and resting). They recommended that all adults (including those with chronic conditions or disability) aim to participate in at least 150 minutes of moderate to vigorous aerobic activity per week, participate in strength training twice per week, and to try to limit sedentary time. The guidelines emphasize that “Every Move Counts” and the importance of muscle strengthening for increasing health and wellness, along with balance activities for people 65 and over to help prevent falls.
The Canadian Society for Exercise Physiology (CSEP) takes an even more integrated approach, with unique recommendations reflecting the importance of balancing physical activity, light activity like walking or wheeling, sedentary time, and good quality sleep. The CSEP 24-Hour Movement Guidelines encourage Canadians to “Make Your Whole Day Matter” and for adults to aim for the following:
- Move more, aiming for at least 150 minutes of moderate (like when you’re starting to breathe heavily but still able to have a conversation) to vigorous (breathing heavy enough that it would be difficult to hold a conversation) aerobic physical activity accumulated over a week, and several hours a day of light activity like standing or slow walking.
- Participate in muscle strengthening activities twice per week.
- Try to limit sedentary time (e.g., watching TV, working at a desk, driving) to eight hours or less and to break up sedentary time as often as possible.
- Aim for seven to nine hours a day of good quality sleep.
Overall, the balance of moving, resting the joints, and getting a good night’s sleep can have great health benefits. Remember that the recommended physical activity time can be broken up into short periods, which can help manage joint symptoms and can also help break up long periods of sitting.
Many of us know that having the knowledge and skill to perform physical activity doesn’t always mean we will do it. And that’s understandable! There are many other factors that come into play, like:
 Motivation: What makes you want or decide to make a change in your lifestyle?
Motivation: What makes you want or decide to make a change in your lifestyle?- Enjoyment: What activities do you like to do? If it’s not something you enjoy, it’s much easier to skip it and harder to stick with it in the long term.
- Opportunity: Is it easy for you to do an activity in terms of when, where, and how? You’ll likely be most successful if your activities are in an environment you’re comfortable in and can readily access, and if you’re doing them at a time of day where you feel you’re most limber and can focus. Timing of taking medications may also come into play.
- Barriers: Are there other barriers to participating, like access to equipment, enough space, or is there a financial burden?
- Symptoms: Some days you’ll feel better than others, in terms of pain and fatigue. How might your activities be modified based on your symptoms? For people with osteoarthritis, long walks or other exercises putting repeated stress on the affected joints might cause too much pain, while people with inflammatory arthritis may be too stiff in the morning to exercise.
There’s no one-size-fits all approach to success when it comes to changing your existing habits and patterns – which is what you’re asking yourself to do as you start a new physical activity routine. Here are some tips that can help:
- Manage your expectations about starting something new, which is rarely easy. Remember that any movement helps.
 Set a goal. Do you want to reduce your sedentary time? Find a new physical activity you like to do? Strengthen your muscles? Become more flexible? Once you know what you want to do, try to identify why you want to do it, and set it as a goal. An example could be, “I want to spend more time in nature (why), so I am going to take a walk outside three evenings a week after dinner (what)”. Goals can help you gain control of your lifestyle. Try to be specific and realistic. Focus on one change at a time.
Set a goal. Do you want to reduce your sedentary time? Find a new physical activity you like to do? Strengthen your muscles? Become more flexible? Once you know what you want to do, try to identify why you want to do it, and set it as a goal. An example could be, “I want to spend more time in nature (why), so I am going to take a walk outside three evenings a week after dinner (what)”. Goals can help you gain control of your lifestyle. Try to be specific and realistic. Focus on one change at a time.- Make a plan. How will you get to that goal, and how will you know if you’re succeeding? Break it down into small, more manageable steps.
- Monitor your progress. Plan to check in with yourself after a few months to reflect on how things are going. Celebrate your achievements, no matter how small, and consider whether any part of your plan needs to change.
- Be kind to yourself. If you lose motivation or have trouble establishing healthy habits, recognize that changing behaviour is hard for everyone. It will take time and you can always return to your goals and plan, adapting them as you learn more about what works for you, and what doesn’t. If you discovered you didn’t like the activity you chose as much as you thought, switch it up and try something else.
- Consider exercising with a friend or monitoring progress with a healthcare or exercise professional if that motivates you to keep on track.
With all the physical activity options that exist, you may wonder where to begin. First, consider what you enjoy doing. It’s much easier to get moving if it’s something you like to do. If you enjoy being outdoors, a nature walk or swim in the lake may be a good option. Or if you prefer to exercise in a group, a yoga class could be a nice way to start. If you dislike certain activities or environments, such as going to a gym or attending a class, then try to find activities that better match your interests.
 As you become more active, remember to take care of yourself. Rest is important, as is being patient with yourself. Changing and establishing new routines is a challenge for most people, and stopping to reassess what works for you doesn’t have to feel like ‘quitting’ – it’s an opportunity to modify your activity plan to suit your needs.
As you become more active, remember to take care of yourself. Rest is important, as is being patient with yourself. Changing and establishing new routines is a challenge for most people, and stopping to reassess what works for you doesn’t have to feel like ‘quitting’ – it’s an opportunity to modify your activity plan to suit your needs.
If possible, you may consider consulting a professional experienced in physical activity and mobility, such as a physiotherapist, occupational therapist, kinesiologist, or other qualified health and exercise professional to help guide you or troubleshoot what isn’t working, or to help increase your activity levels in ways that interest you.
To help you choose activities you enjoy, here are some articles and resources for inspiration. You’ll also find articles on self-care such as supporting good sleep and maintaining your energy.
Arthritis and physical activity
Articles
- The right exercise mix: Understanding the different kinds of exercise—flexibility, strength and endurance—and how they work together as part of an arthritis physical activity plan.
- Choosing arthritis-friendly activities: Choose low- and no-impact exercises that won’t cause further wear to your already painful joints.
- Starting fitness: Expert tips on how to start exercising to help decrease arthritis pain, including information on setting goals, understanding what pain means, posture and food and water.
Videos
How to get active again to help manage arthritis |

Arthritis and movement |

The role of physical activity when managing arthritis |

Managing Arthritis with Physical Activity and Assistive Devices |
Physical activity by arthritis type
Articles
- Osteoarthritis self-management: The first line of treatment for osteoarthritis (OA) involves a number of steps you can take on your own under the guidance and supervision of a healthcare professional.
- 7 ways to deal with osteoarthritis back pain: An overview of coping strategies for osteoarthritis-related back pain, including exercise, weight loss, shoe choice, posture, chiropractic care and strengthening and stretching.
- Managing gout: Strategies for managing gout, including food and drink choices, exercise and medication therapies.
Video
Managing physical activity with inflammatory arthritis
The Movement for All Lab’s I START Toolkit and exercise videos for strength training for people with rheumatoid arthritis (funded in part by Arthritis Society Canada)
Types of physical activity
Articles
- Arthritis and walking: Arthritis Society physiotherapist Ingrid Beam presents simple tips to help people with arthritis incorporate walking into their activities, as it is one of the best ways to help strengthen joints and improve mobility.
- Arthritis on the move: Nordic walking: Staying active is a vital part of living well. For many people with arthritis, Nordic walking can be a safe and fun way to get fit, stay active and retain your mobility.
- What is forest therapy: Forest therapy, also known as forest bathing, is about mindfully spending time outdoors, especially in a wooded setting, with potential mental and physical health benefits.
- Is yoga for arthritis right for you? Discover 6 reasons why yoga for arthritis may be right for you.
- Water therapy and arthritis: Find out how hydrotherapy, also known as water therapy or aquatherapy, can help improve arthritis pain, joint tenderness and balance, in a social fun setting.
- Top 7 tips for golfing with arthritis: Tips for golfers living with arthritis, including exercises, gear, and warm up and cool down routines, from a PGA golf coach and an Arthritis Society Canada physiotherapist.
Videos
GLA:D + Movement |

Is yoga for arthritis right for you? |

Tai Chi to Help Arthritis |
Self-care and mental health
Articles
- 10 things to do before you go to sleep: Living with chronic pain can make it hard to get a good night’s sleep. Here are some pro tips to getting your Z’s if you’re living with arthritis.
- 10 tips for managing morning stiffness in your joints: Painful and stiff joints can make mornings difficult for people living with arthritis. Whether you have osteoarthritis or a form of inflammatory arthritis, these tips will help.
- Pain self-management tools: An important part of arthritis pain control is self-management. This refers to activities and supports that you can use on your own to reduce joint pain.
Finding new ways to engage in physical activity or exercise can be an overwhelming process, especially if you’re also navigating arthritis symptoms. We’ve put together a curated list of our physical activity and exercise resources and videos for you to follow along with.
Whether you’re a beginner or a physical activity enthusiast – we have something for you.
| 20-Minute warm-up for the joints
|
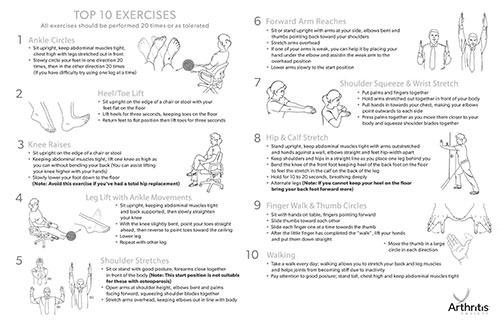
Top 10 arthritis exercises
In this PDF, you will find out 10 Arthritis friendly exercises you can do almost anywhere. |
Yoga for arthritis: introduction to breathing
|
| Beginner’s chair yoga for arthritis
|
Seated and standing yoga
|
Floor yoga for arthritis
|
| Standing yoga with props
|
Restorative yoga in bed
|
A Warrior Series
|
| Yoga for Rheumatoid Arthritis
|
Tai Chi to Help Arthritis
|
Arthritis Advice: Hand Exercises
|
| Arthritis Advice: Neck & Back Exercises
|
Arthritis Advice: Knee Exercises
|
Introduction to Exercise for Osteoarthritis
| 1. Introduction to osteoarthritis and exercise | 2. Exercises for osteoarthritis of the hip and knee | 3. Exercises for osteoarthritis of the shoulder |
Exercises for osteoarthritis of the hip and knee
| Part 1 : Introduction – Exercises for Arthritis of the Hip and Knee | Part 2 : Starting an Exercise Program | Part 3: Exercises – Hip & Abductor Muscles (Glutes) |
| Part 4: Exercises – Quadricep, Hamstring and Calf Muscles | Part 5: Exercises – Trunk/Core Muscles | Part 6: Exercises – Stretches |
Exercises for osteoarthritis of the shoulder
| Part 1: Introduction to Exercise for Osteoarthritis of the Shoulder | Part 2: Exercises – Shoulder Range of Motion and Stretching | Part 3: Exercises – Shoulder Strengthening (Rotation) |
| Part 4: Exercises – Shoulder Strengthening (Flexion, Abduction, and Extension) | Part 5: Exercises – Scapular Muscle Stabilization |
Contributors
This physical activity resource was developed and last reviewed in November 2023 with expert advice from:
Dr. Jasmin Ma, PhD, P.Kin, CIFT (ACSM)
Assistant Professor of Teaching, School of Kinesiology, University of British Columbia
Clinician Investigator, Arthritis Research Canada
with support from
Caitlin Chiu
School of Kinesiology, University of British Columbia